-
Now Offering Limited Time Dental Promotions
We are committed to offering customized, affordable care. Take advantage of our special offers!
Offers Expire: April 30th, 2024 Book Your Appointment

We Care About YOU, Your Smile & Your Health
Welcome to Radiant Family Dentistry, your trusted Scottsdale family dentist! Dr. Christine Chan and her team provide compassionate and comprehensive dental treatments, including preventative, restorative, and cosmetic dental services. Our office is designed to serve all of your needs and is conveniently located to serve those living and working near Scottsdale, AZ!
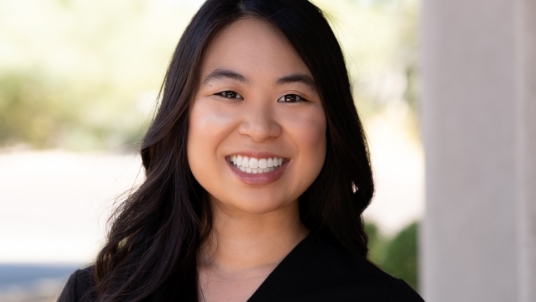
Dr. Christine Chan
My name is Dr. Christine Chan and it is with great pleasure to introduce myself and express both my gratitude and excitement in providing exceptional dental care for you and your family.
Your Comfort Is Our Priority
At Radiant Family Dentistry, your comfort comes first! Our team is here to ensure you leave our office feeling confident in your smile. To achieve this, our dental practice focuses on restoring and maintaining optimal oral health through gentle, advanced techniques. Our practice offers a variety of unique amenities to help both kids and adults stay comfortable, including headphones, soft blankets, and pillows, free Wi-Fi, complimentary hand masks and lip balms, kid-friendly toys, and more. We're here to help patients of all ages feel right at home.

Your Preferred Invisalign® Provider
As an Invisalign Preferred Provider, our dentist has the expertise to discreetly straighten smiles of all ages. Invisalign orthodontics provide fast, effective results, with comfortable aligners that allow you to reach your smile goals with ease!
We Offer a Comprehensive Service List
At Radiant Family Dentistry, we take pride in the skill, experience, and commitment of our team.
Dr. Chan utilizes a unique combination of science and artistry to redesign and restore patients' smiles, with a variety of advanced dental services designed to detect, diagnose, and treat potential oral health issues early on. Our advanced dental services include preventive exams, Invisalign clear braces, dental veneers, teeth whitening, emergency dentistry, same-day appointments, permanent dental implants, crowns and bridges, removable dentures, periodontal therapy, custom mouth guards, and much more!
-
Emergencies
At Radiant Family Dentistry, we are here to provide the comfort and care needed during emergencies.
-
Crowns & Bridges
Cavities or tooth loss? Our luminous crowns and bridges will seamlessly blend in with the rest of your smile.
-
Dental Implants
Restore your smile from the damaging effects of tooth loss with state-of-the-art dental implants.
-
Invisalign
Straighten your teeth with discreet, removable Invisalign clear aligners. No dietary restrictions required!
-
Dentures
Eat and drink with confidence! Our dentures are hand-crafted to fit each patient's unique smile.
-
All Services
We pour honesty, quality, & top-notch care into every service we provide at our Scottsdale, AZ dental office.
Flexible Financing for the Smile of Your Dreams
Radiant Family Dentistry is committed to providing comprehensive dental care to the entire family! Whether your dental needs are simple or complex, our goal is to provide you with the quality dentistry you want and deserve. Dr. Chan and her team achieve this by offering financial consultations, flexible financing options, and complete support to all of our patients so you can focus on the quality of your dental care, not the investment.

Smile with Confidence!
We provide comprehensive dental care to all. Whether your case is simple or complex, our team is committed to restoring your dental health every step of the way. If you have any questions about our service list, office amenities, or your dental investment, give us a call to get the answers you need.
Welcome to Radiant Family DentistryAssociations & Accreditations
Dr. Christine Chan is a member of the American Dental Association, the Arizona Dental Association, and the American Academy of Clear Aligners.
Experiencing an Emergency? Give Us a Call:
(480) 462-0639Visit Us Today
7595 E McDonald Dr Ste 110, Scottsdale, AZ 85250 (480) 948-1255- Monday:
- 8:00AM - 5:00PM
- Tuesday:
- 8:00AM - 5:00PM
- Wednesday:
- 8:00AM - 5:00PM
- Thursday
- 8:00AM - 5:00PM
- Friday:
- 8:00AM - 12:00PM
Visit Us Today
7595 E McDonald Dr Ste 110, Scottsdale, AZ 85250 (480) 948-1255- Monday:
- 8:00AM - 5:00PM
- Tuesday:
- 8:00AM - 5:00PM
- Wednesday:
- 8:00AM - 5:00PM
- Thursday
- 8:00AM - 5:00PM
- Friday:
- 8:00AM - 12:00PM